HOW AND WHERE KIDNEY STONES OCCUR
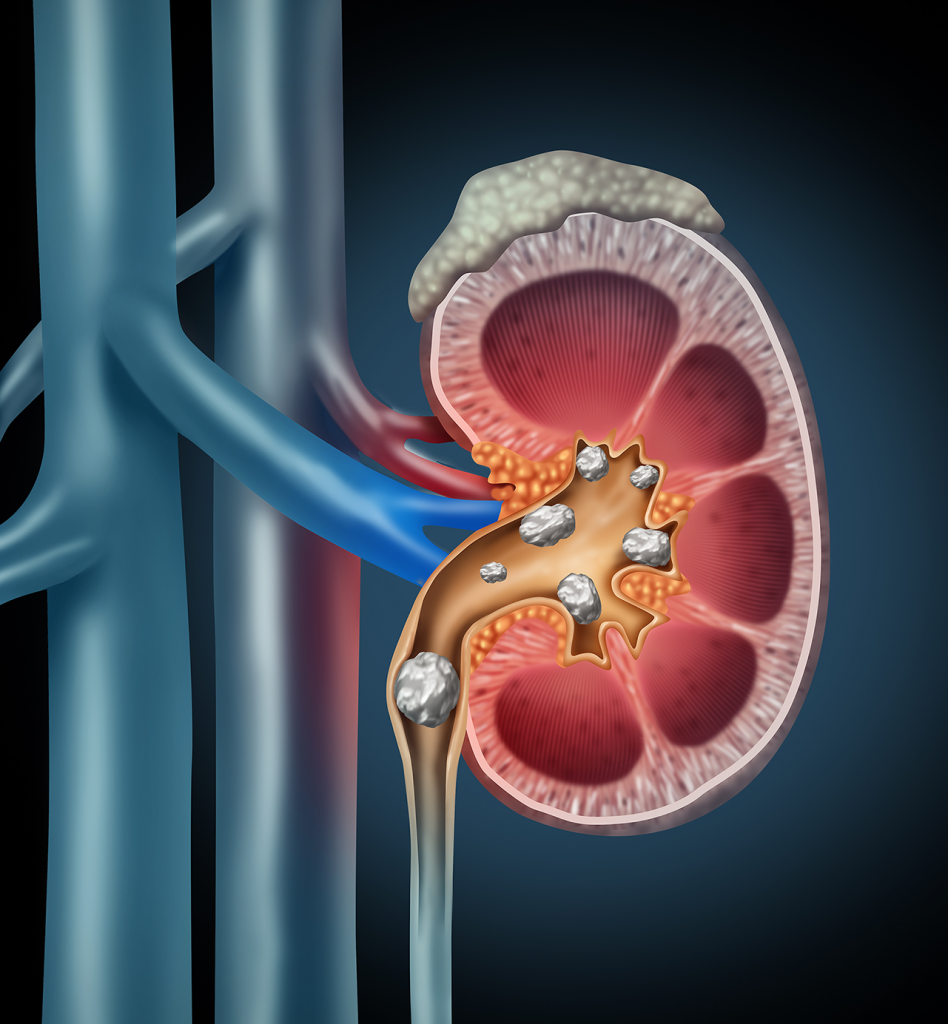
Most urinary stones (urolithiasis in medical terms) arise as a result of a change in the natural balance of minerals and water in the urine. They consist of salt and minerals in the urine, which stick together and form small clots. The stones are rarely larger than a grain of rice, but they can grow to several centimeters in diameter and in some cases they even fill the entire renal collecting system.
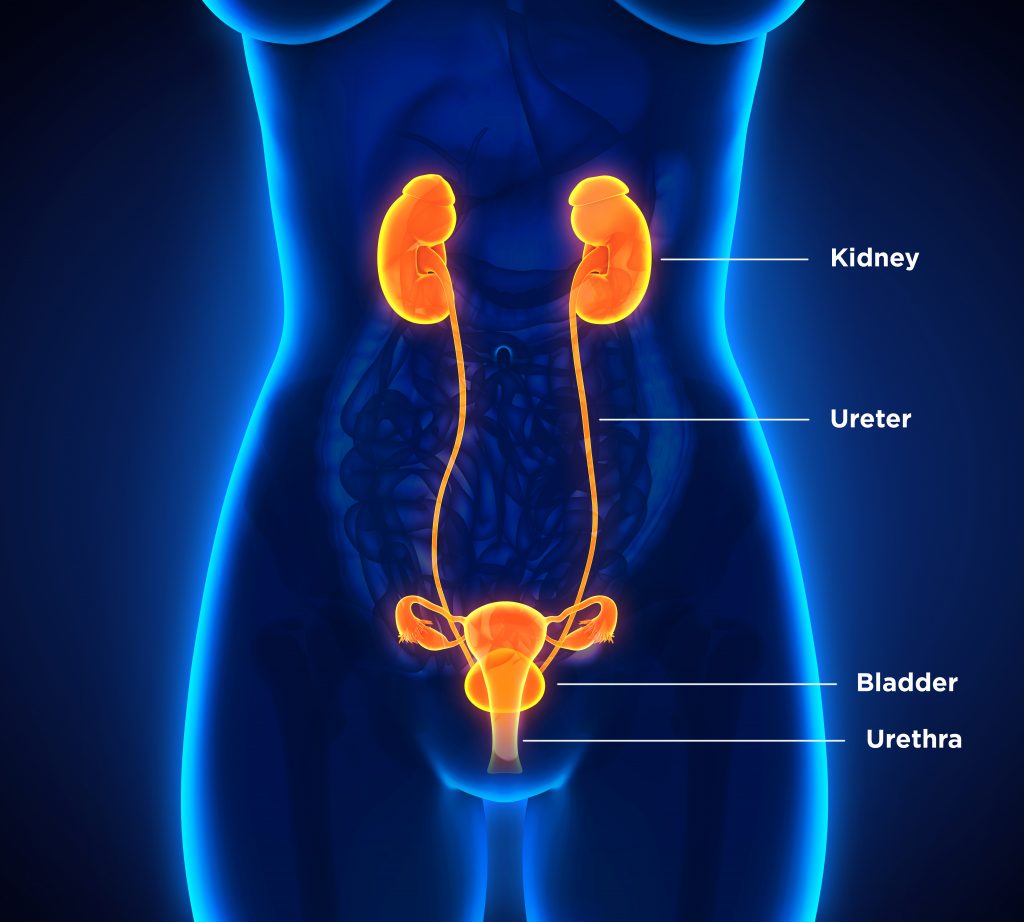
They can stay in the kidneys or exit the body through the urinary tract. The urinary tract is the system that generates and excretes urine. It comprises the kidneys, the ureters (which connect the kidneys to the bladder), the bladder and the urethra, through which urine is transported from the bladder out of the body. Depending on the diagnosed condition, a distinction is made between kidney, urinary and bladder stones. Doctors distinguish between the type of salt that the stone comprises, for example:
- Calcium oxalate stones (70-75%) [1, 2]
- Uric acid stones (up to 10%) [1, 2]
- Infectious stones, e.g. “Struvite stones” consisting of magnesium ammonium phosphate (approx. 10-15%) [1-3]
Factors that can change the balance of substances in the urine and are therefore a common cause of kidney and urinary stones include the following:
- Insufficient water intake, which can result in salts and minerals sticking together to form small stones. [2, 4]
- A protein- or sodium-rich diet [5, 6]
- Frequent urinary tract infections [2, 4]
- Metabolic syndrome, obesity, diabetes and gout [1, 7-10]
- A regulatory disorder of the parathyroid glands (hyperparathyroidism) [1, 2, 4]
- Bowel surgery, gastric bypass and chronic bowel disease (Crohn’s disease) [1, 2, 4]